Cervicitis: Definition, Causes, Symptoms and Treatment
Gynecologists refer cervicitis – an inflammation which affects uterine cervix – to a quite common disease of the female genital sphere, because throughout life at least once 50% of women suffer from this disease.
Infection appears in the uterine cervix, which serves as a protective barrier for infectious microorganisms; inflammation is divided into several stages. In two-thirds of cases, the disease occurs during the fertile age.
Inflammation Causes
Based on the fact that the disease is very common, it may be caused by various reasons:
- vaginal infection or sexually transmitted diseases (chlamydiosis, gonorrhea, trichomoniasis and others);
- candidiasis;
- herpes simplex virus (genital herpes);
- human papillomavirus;
- uterine cervix birth injuries – mechanic damage caused by unprofessionally conducted abortion, biopsy of the uterus lining, artificial cervical dilatation using special tools or fixation or removal of the contraceptive uterine coil;
- early sexual debut – uncontrolled sexual behavior, several sexual partners; poor personal hygiene;
- an allergic reaction to latex or spermicides and others.
Symptoms and Signs
The first symptom of cervicitis can be more intense vaginal discharge, starting immediately after the end of menstruation. However, because of weak intensity, it is very difficult to reveal the disease at this stage without gynecological examination. The main symptoms include:
- itch;
- burning and redness of externalia;
- burning with urination or urethralgia;
- profuse discharge;
- bleeding between menstruations;
- dyspareunia;
- slight blood-tinged discharge or bleeding immediately after sexual intercourse;
- uterine colic or lumbar pain (sometimes they appear only during sexual intercourse);
- mild nausea, body temperature increase, dizziness and florid uterine colic (occur when the infection spreads);
- hyperemia and cervical canal external opening edema, combined with endometrium montanum and slight hemorrhaging or ulceration (revealed at examination).
 It should be noted that depending on pathogen type and the general state of immunity cervicitis may have different manifestations. Thus, for instance, cervicitis caused by gonorrhea usually has acute course, its signs are florid. On the contrary, at chlamydial infection symptoms are less prominent. Cervicitis, caused by herpes, is characterized by loose bright red uterine cervix with ulcerations. In presence of trichomoniasis, the disease occurs with slight hemorrhaging on the uterine cervix and abnormal cells in the smear. Human papillomavirus on the background of cervicitis often leads to condyloma formation and extensive uterine cervix ulceration.
It should be noted that depending on pathogen type and the general state of immunity cervicitis may have different manifestations. Thus, for instance, cervicitis caused by gonorrhea usually has acute course, its signs are florid. On the contrary, at chlamydial infection symptoms are less prominent. Cervicitis, caused by herpes, is characterized by loose bright red uterine cervix with ulcerations. In presence of trichomoniasis, the disease occurs with slight hemorrhaging on the uterine cervix and abnormal cells in the smear. Human papillomavirus on the background of cervicitis often leads to condyloma formation and extensive uterine cervix ulceration.
Cervicitis is dangerous because of mild coarse it can completely invisible. And if at acute course it was not revealed and, as a consequence, not cured, the disease transforms into chronic stage. At chronic cervicitis, major inflammation signs (edema and hyperemia) are less prominent.
However, without treatment further on, the inflammation will spread to surrounding uterine cervix tissues and glands, causing cyst encapsulation and infiltrate formation and cervical induration appears. Therefore, do not neglect regular medical examinations, since it’s extremely important for your health and ability to conceive and have healthy children.
It should be pointed out, that pathogens can be defined according to the urethra or vagina discharge specifics. For example:
- At cervicitis on the background of gonorrhea, discharge obtains yellow color with pus. At chlamydiosis or mycoplasmosis discharge changes are less prominent. It usually is transparent or white, may have a yellow tint.
- If cervicitis is caused by urinogenital trichomoniasis, the discharge will be foamy.
- If the cause is candidiasis, discharge is the same as at vaginal thrush. It is white and thyroid.
Types of cirvicitis:
- acute;
- chronic;
- purulent;
- atrophic;
- viral;
- bacterial;
- cystic;
- nonspecific.
Diagnostics
Cervicitis is often asymptomatic, so in most cases, the disease is diagnosed only during routine medical examinations or visiting gynecologist with other diseases.
The point of diagnostics is to define inflammatory infection cause, namely pathogen determination contribute to effective treatment. Accurate diagnosis is established on the basis of the following results:
- uterine cervix surface examination using gynecological speculum;
- extended colposcopy, which allows registering even slight changes in cervical epithelium (vascular slings, swollen mucosa, ectopia or anabrosis, hyperemia, and inflammation cause) and on this basis to determine the effectiveness of further treatment;
- laboratory tests (bacterial inoculation for sensitivity to antibiotics and flora, smear, PCR-based diagnostics, vaginal fluid pH-metry, etc.);
- special diagnostics methods (enzyme immunoassay, DNA-probe, etc.).
Treatment
For successful treatment firstly it is necessary to determine and eliminate disease pathogen and predisposing factors (metabolism, hormone, immune disorders). Therefore, cervicitis treatment type in many aspects depends on inflammation caused.
After diagnostics and causative agent, definition gynecologist prescribes a number of drugs that most effectively and in short time help to get rid of the infection. Moreover, during the entire treatment period, it’s required to undergo laboratory tests and colposcopy for monitoring recovery dynamics.
Besides, patients are recommended physiotherapy together with drug therapy that enhances host defense. At nonspecific cervicitis often appointed by vaginal douche and suppositories.
It is also worth noting that to avoid re-infection it’s advised to conduct treatment of your sexual partners.
Treatment with Ampicillin
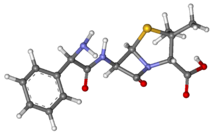
Ampicillin (Ampicillinum) is a semisynthetic antibiotic used for treating various infectious respiratory tract (pneumonia, bronchial pneumonia, sore throat), urinary tract, gastrointestinal tract diseases and hepatopathy. It was first released in 1961 by British company «Beecham».
Canadian Pharmacy Ampicillin is a crystalline white powder with a bitter taste; stable in the acidic medium; slightly soluble in water, practically insoluble in alcohol. It is obtained by 6-amino penicillanic acid acidulation with aminophenylacetic acid.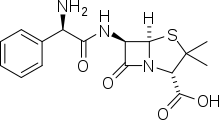
The drug is not degraded in stomach acidic medium, is well absorbed when taken orally. It inhibits bacterial cell wall synthesis.
Active against gram-positive (alpha- and beta-haemolytic streptococcus, Streptococcus pneumonia, Staphylococcus spp., Bacillus anthracis, Clostridium spp., moderately active against Enterococcus, including Enterococcus faecalis), Listeria spp., and gram-negative (Haemophilus influenzae, Neisseria meningitidis, Proteus mirabilis, Yersinia multocida (former Pasteurella), many species of Salmonella spp., Shigella spp., Escherichia coli) microorganisms, aerobic nonspore-forming bacteria.
Ineffective against penicillinase-producing strains of Staphylococcus spp., all strains of Pseudomonas aeruginosa, most strains of Klebsiella spp. and Enterobacter spp.
Ampicillin potentiates oral anticoagulants.
Contraindications:
- hypersensitivity (including other penicillins, cephalosporins, carbapenems);
- infectious mononucleosis;
- lymphatic leukemia;
- hepatism;
- colitis, caused by antibiotics;
- lactation period;
- children’s age (up to 1 year).







